Treatment of Obstruction
Traditional Surgical Treatments
Nasolacrimal Duct Obstruction (NLDO) and Surgical Treatment Techniques
Nasolacrimal duct obstruction (NLDO) poses a common challenge in ophthalmology, affecting both pediatric and adult patients. This condition results from the blockage of the nasolacrimal drainage system, leading to epiphora, mucopurulent discharge, and discomfort. Various surgical techniques address NLDO, each with distinct benefits. Let us explore these modalities in detail:
1. Probing and Irrigation
Indications: Probing and irrigation serve as initial interventions, especially in infants. When conservative management (massage and topical antibiotics) fails, probing becomes essential.
- Procedure:
- The ophthalmologist gently inserts a probe through the punctum, navigating it through the lacrimal drainage pathway.
- The goal is to break down adhesions or blockages.
- Probing is often performed under local anesthesia.
- Benefits:
- Effective in many cases.
- Minimally invasive.
- Provides immediate relief in appropriately selected patients.
2. Balloon Dacryoplasty (DCP)
Overview: Dacryoplasty involves balloon catheter dilation and is performed under general anesthesia.
- Procedure:
- A deflated balloon catheter is inserted into the nasolacrimal duct.
- Inflation dilates the obstructed area, widening the drainage passage.
- Ideal for congenital NLDO cases where probing and irrigation have failed.
- Benefits:
- Minimal scarring.
- Expedited healing.
- Reduced bruising and swelling.
|
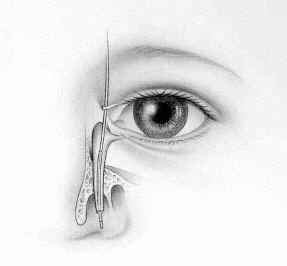
STEP 1:
The LacriCATH ® balloon catheter (shown in the picture) is inserted through an opening in the corner of the eye and down into the tear duct .® balloon catheter (shown in the picture) is inserted through an opening in the corner of the eye and down into the tear duct .balloon catheter (shown in the picture) is inserted through an opening in the corner of the eye and down into the tear duct .
|
 |
| |
| STEP 2:
The balloon catheter is inflated with sterile water to dilate the tear duct for a period of 90 seconds. It is then deflated, and reinflated for 60 seconds.
|
 |
| |
| STEP 3:
The balloon catheter is then repositioned slightly higher in the duct and inflated twice as in step 2.
|
 |
The balloon catheter is then deflated and removed.
 |
 |
|
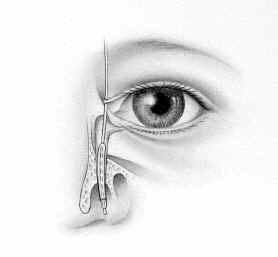
Here you can see the balloon as it is inflated within the nose
|
3. Endoscopic Dacryocystorhinostomy (Endoscopic DCR)
Indications: Persistent NLDO cases unresponsive to conservative measures.
- Procedure:
- Performed under general anesthesia.
- An endoscope provides direct visualization to create a new drainage pathway between the lacrimal sac and nasal cavity.
- Bone and tissue removal establish a direct connection.
- Effective in both adults and children.
- Benefits:
- Better illumination and magnification.
- Potentially shorter surgical time.
- Minimal scarring.
- Early treatment option for acute dacryocystitis.
- Details
-
This minimally invasive surgery is performed to treat nasolacrimal duct obstruction, which can cause excessive tearing, recurrent infections, and discomfort.
- Patient Preparation:
- The patient is positioned supine (lying on their back) under general anesthesia (usually) or local anesthesia with sedation (special circumstances).
- Sterile drapes are placed to maintain a sterile field.
- Visualization and Access:
- An endoscope (thin, flexible tube with a camera) is inserted into the nasal cavity to visualize the nasolacrimal duct and surrounding structures.
- The middle turbinate is reflected to reveal the middle meatus space adjacent to the lacrimal bone that abuts the lacrimal system. Next, local anesthetic and vasoconstrictors are applied to the mucosal tissues to numb the eyelids and the intranasal area of the middle meatus, lacrimal bone, and the lateral nasal wall.
- Identification of the Lacrimal Sac:
- The surgeon identifies the lacrimal sac (the dilated section of the nasolacrimal track), using small probes inserted into the eyelid portion of the lacrimal system. The sac is often obstructed due to scar tissue, stones, inflammation, infection or other factors.
- Creation of a Bony Ostium:
- Using specialized instruments and the camera for direct visualizaion, the surgeon removes a small portion of the adjacent nasal bone (usually the anterior part of the maxillary bone).
- This creates a bony ostium (opening) between the lacrimal sac and the nasal cavity.
- Mucosal Flap Creation:
- The nasal mucosa (lining of the nasal cavity) is carefully elevated over the bony ostium.
- A mucosal flap is created, serving as a lining for the new drainage pathway.
- Connecting the Lacrimal Sac to the Nasal Cavity:
- The surgeon opens the lacrimal sac and connects it to the newly created bony ostium.
- This allows tears to bypass the blocked nasolacrimal duct and drain directly into the nasal cavity.
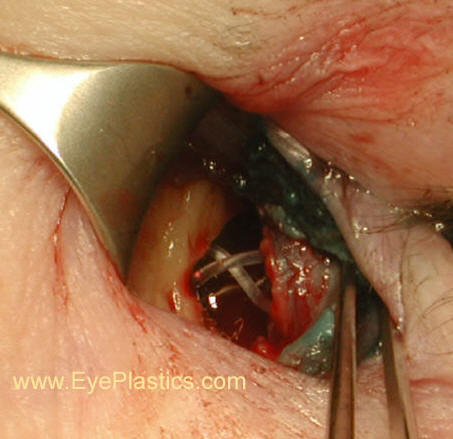
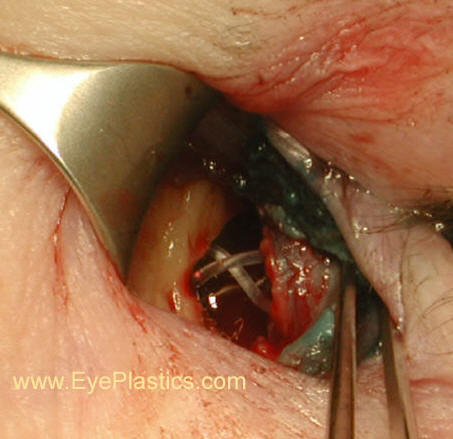
- Placement of a Silicone Stent or Tube:
- To maintain the patency of the new drainage pathway, a silicone stent or tube may be inserted into the lacrimal sac and through the ostium.
- The stent helps keep the pathway open during the healing process and is removed easily in the office approximately 3 months after surgery.
- Closure and Recovery:
- Dissolvable nasal packing may be used to control bleeding.
- Patients are monitored in the recovery room discharged to home the same day.
- Postoperative Care:
- Oral Antibiotics, eyedrops, and nasal decongestant are prescribed.
- Follow-up appointments are scheduled to monitor healing and stent removal.
- Outcome:
- Endoscopic DCR has a high success rate in relieving symptoms of tearing and improving tear drainage.
- Patients typically experience minimal pain and faster recovery compared to traditional external DCR, with the added benefit of direct visualization into the nasal passage and lacrimal track at all times, and no visible external scarring.
In summary, endoscopic DCR precisely restores tear drainage by creating a new pathway from the lacrimal sac to the nasal cavity. It offers significant benefits for patients suffering from nasolacrimal duct obstruction.
4. Silicone Stent Intubation
Indications: Used in refractory NLDO cases.
- Procedure:
- A silicone stent maintains patency by remaining in the nasolacrimal duct for several months.
- Suitable for both congenital and acquired NLDO.
- Benefits:
- Continuous drainage support.
- Can be combined with other techniques.
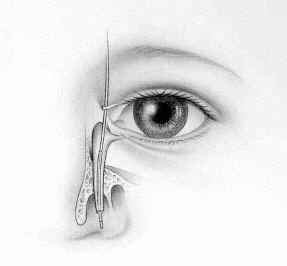
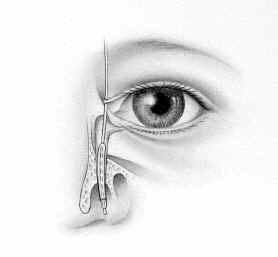
5. External Dacryocystorhinostomy (External DCR)
Indications: Used when endoscopic approaches are not feasible or unsuccessful.
- Procedure:
- Performed under local or general anesthesia.
- An oculoplastic surgeon creates an external incision near the medial canthus.
- Directly connects the lacrimal sac to the nasal cavity.
- Potential complications include visible scars and prolonged healing.
- Benefits:
- Effective for both congenital and acquired NLDO.
- Allows direct visualization of the lacrimal sac.
Movies of Surgical Lacrimal Duct Procedures
Lacrimal Stents
CDCR / JONES tube / PG tube
If the "tear duct" obstruction is beyond repair, It might be necessary to surgically implant an artificial "tear duct" behind the inner corner of the eyelids to drain the tears into the nose. The artificial "tear duct" is made of Pyrex glass and is called a "Jones tube." or Putterman-Gladstone (PG) tube.
These might be purchased at Gunther Weiss Glass Science, located in Portland Oregon. 503-644-3507
Dacryocystorhinostomy surgery provides relief to millions of people every year who suffer from tear duct problems ranging from collapsed tear ducts and excessive tearing caused by accident or injury, birth defects or environmental strain. Left untreated, patients might experience swelling, infections, increased swelling, tearing ("wet eye") and severe pain.
In 1961, Lester T. Jones and Gunther Weiss paired up to develop a solution for tear duct problems. They developed highly specialized glass tubes (called "Lester T. Jones Tear Duct Tubes") designed for insertion into the nasolacrimal duct. The body develops scar tissue around the tube, which holds it in place, forming a new permanent tear duct.
Gunther Weiss Scientific Glass Blowing Company offers Lester T. Jones Tear Duct Tubes in a variety of lengths and diameters to address most patient needs. In adds to, tubes can be custom-fabricated to accommodate unique angles and sizes
In summary, individualized management of NLDO involves thorough evaluation and informed decision-making. Whether probing, balloon dacryoplasty, endoscopic DCR, or silicone stent placement, ophthalmologists strive to restore tear drainage and improve patients’ quality of life.